If you’re reading this, it’s likely you’ve been diagnosed with gestational diabetes (GD). Or, maybe you’re pregnant and heard about GD, or you’re about to take the GD glucose test, and are curious to learn more about GD in general. Alternatively, you might not be pregnant at all, but still interested in learning more about GD and various options. Regardless of your situation, I hope this post provides some helpful information related to nutritional guidance in light of GD.
In this post, I wanted to share a little about an experience I had when I was pregnant with my son. While I didn’t have GD myself, I sat in a room with others who had been diagnosed with GD and heard the nutritional guidance they were supposed to start following. The advice seemed contraindicative to the condition they were trying to manage and it made me want to learn more, in the hopes that I could share that information with other pregnant mamas.
Gestational diabetes can be a scary diagnosis for an expecting mother. A quick Google search yields an overwhelming amount of information about the serious risks for both baby and mama that can be connected to the condition. If you’re reading this as an expecting mama who’s been diagnosed with GD, please know that I can definitely imagine the range of emotions you’ve experienced. I encourage you to read about my experience, and then to check out the resources I reference below for effectively managing GD. You CAN most definitely have a full term, healthy pregnancy and the childbirth experience you’re hoping for with GD. Many women do!
Here’s the story:
When I was pregnant with my son in 2019, and it was time for the standard gestational diabetes test, I asked my doctor to let me monitor my blood glucose levels for two weeks instead of drinking the glucola. My doctor at the time was willing to go this route and asked that I attend the hospital’s course on gestational diabetes, where I would learn the proper way to use a glucometer. A glucometer is the little device that pricks your finger so you can measure your blood sugar levels.
I was one of about eight pregnant women attending the 2-hour class. The instructors were a nurse and a registered dietician from the hospital and they walked us through all things GD. I learned to use a glucometer like I planned. I also learned how women with gestational diabetes were instructed to manage their diabetes. Over the years, my mother and I have done quite a bit of research on nutrition, so we know a thing or two about the effects of elevated blood sugar on long term health. We also know a lot about the foods and methods that help maintain proper blood sugar levels, and those that don’t.
It’s safe to say I was shocked by the nutritional tips being given to my fellow pregnant mamas.
Before I keep going, I should mention that nutrition is often a controversial topic. Many dietitians and nutritionists were taught and still operate from outdated information about how certain food groups or specific foods support or detract from our health. It takes years and sometimes decades to change nutritional guidelines at the national level and in our university and other school curriculums.
That being said, there are also nutrition professionals who are very informed on the latest nutritional information and studies available today. The professional I mention below is one of those individuals who uses scientific evidence and her own clinical experience to provide nutritional guidance for pregnant women with and without GD.
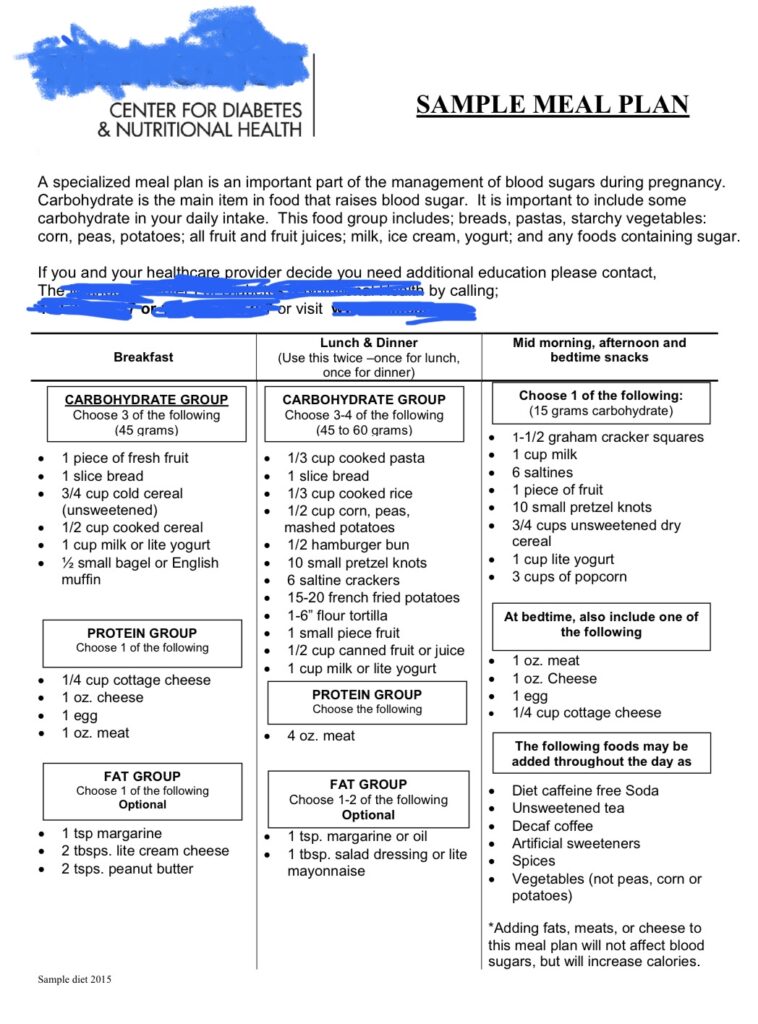
Keeping in mind that these nationally-accepted and promoted nutritional guidelines are often outdated by many years, let’s take a look at the sample meal plan the course instructors handed out to each of us:
You’ll notice that women are encouraged to eat 45 grams of carbohydrates at breakfast, 45-60 grams of carbs at both lunch and dinner, and another 15 grams of carbs for mid-morning, afternoon and bedtime snacks (which would be 45g total). That means pregnant women are being instructed to eat 180-210g of carbs per day! That is a lot of carbs for someone whose body is experiencing heightened blood sugar levels and insulin resistance.
The other problem is that the types of carbs suggested in the meal plan are essentially “empty” carbs that will provide very little nutritional benefit.
Bagels, English muffins, bread, graham crackers, saltines, pretzels and cereal are mostly made with processed white flour. Fruit juice and high glycemic whole fruits are very high in sugar (aka carbs) as well. These foods raise blood sugar extremely quickly. They also leave a person hungry again in just a couple hours if they’re the main part of their meal or snack. A more ideal suggestion would be a total lower carb count, and promoting complex, starchy carbohydrates (i.e. sweet potato, carrots, etc.) over simple carbs (i.e. comprised of flour or sugar).
The remaining suggestions in the diet plan are just as worrisome. Let’s take a closer look:
The meal plan promotes eating margarine – a highly processed food made with inflammatory seed oils. Grass-fed butter and extra virgin olive oil would provide substantially more health benefits.
The plan also allows diet soda and artificial sweeteners. These are lab-created, artificial ingredients. In addition, studies show that consuming either of these items promotes overeating. One goal of managing gestational diabetes is to eat intuitively based on your body’s cues so that you don’t eat more than your body truly needs. Consuming foods that trick your body into thinking it wants more food makes it extremely challenging to eat intuitively.
In addition, consuming artificial sweeteners long-term has been shown to produce elevated blood glucose levels and insulin resistance. That means these items are still raising blood sugar, even though there’s no “real sugar” in them!
The meal plan suggests about 10oz of protein (roughly 79g) per day. Recent research has found that pregnancy requires a higher protein intake than previously thought and what the institutional guidelines suggest. Current research suggests a woman who weighed 150lbs pre-pregnancy, really needs a MINIMUM of 80g of protein in early pregnancy and 100g in late pregnancy.
The meal plan is void of any mention of vegetables. Delicious veggies prepared or eaten with high quality fats promotes proper nutrient absorption and can take the place of a bagel or other empty carb that provides little nutritional value and leaves you hungry sooner.
The last line in the meal plan is the real kicker: “Adding fats, meats or cheese to this meal plan will not affect blood sugars, but will increase calories.” Fats and proteins do affect blood sugar, but in positive ways! They help blunt the rise in blood sugar that would normally occur because of the ingested carbs. That’s why it’s wise to always eat high quality fats and protein alongside carbohydrates.
Yes, they may increase calories, but they contain far more nutrients and minerals critical for growing a baby! Since protein and fat make you feel fuller for longer, this means a pregnant woman consuming pasture-raised meats and eggs and high quality fats will end up less likely to overeat overall. Considering what I just shared about protein requirements, it would be far better to promote increasing meat consumption and decreasing carb consumption.
This information was given to me back in 2019. It’s possible the information that’s given to women with GD today has improved and I would welcome any examples currently or recently pregnant women would be willing to share with me from their experience! You can email me here.
So where would one go to find the latest nutritional information for a healthy pregnancy?
My favorite resource for pregnancy nutrition based on current evidence and science is Lily Nichols, RDN, CDE. I often share insights from her in-depth blogs on GLAMamas social media accounts and reference her work in our blogs when applicable.
Every single person benefits from a real, whole foods diet. If you’re trying to conceive, pregnant or pregnant with gestational diabetes, you and your baby will benefit even more!
Lily provides some fantastic free resources on her website.
If you are trying to conceive or are currently pregnant, Lily’s book is awesome.
If you have gestational diabetes, Lily has a book specifically for managing GD with a real food approach.
I highly recommend you check her info and books out!
A few other things to consider if you have gestational diabetes:
Physical activity plays a crucial role in managing blood glucose levels. Taking a 10-30 minute walk after each meal will help blunt elevation of blood sugar levels. Physical activity is also incredibly beneficial for preparing your body for the intense act of giving birth, so it’s important for all pregnant women to stay as active as they can up until labor starts. Plus, it’ll make you feel better and promotes ideal weight gain and management, too!
Your mindset also matters. Just because you’ve been diagnosed with GD, doesn’t mean you’ll experience any of the risks you might have learned or heard about. Instead of fixating on GD or any of those risks, focus purely on what you WANT to happen. As soon as an worrisome or negative thought creeps in, stomp it out with a positive one instead. Here are examples of thoughts that focus on what you WANT to happen, instead of what you don’t want to happen:
I will give birth to my perfectly healthy baby.
My body knows exactly what to do.
I feed my body and my baby with wonderful, nourishing foods.
My body is amazing and miraculous!
I love to move my body often and throughout my day!
I crave nourishing and nutritious food!
I will birth my baby full-term.
The birth of my baby will be beautiful, calm, safe and serene.
You’ve got this, mama!
One other thing to note is that breastfeeding greatly reduces your risk of developing type 2 diabetes post-pregnancy (something that women with GD are at a higher risk of experiencing).
I am not a medical doctor. I am your pregnancy, birth, breastfeeding and motherhood advocate! I aim to supply information to help other women support their health and their children’s health. You will need to consult with your doctor to come up with an approach that works best for you. From my knowledge and experience related to the topics discussed here, I leave you with this GD “formula” for success:
Proper Nutrition + Physical Activity + Positive Mindset (visualizing your ideal outcome) + Breastfeeding = Your BEST outcome for GD and ongoing diabetes risk post-pregnancy
If you know anyone else who would benefit by reading this blog, please be sure to send it their way!
Active-ist for your health (and your baby’s!),
Brianna
This post contains affiliate links and we may earn a small commission when you click on the links, at no additional cost to you. As an Amazon Affiliate, we earn from qualifying purchases. Each of these items we’ve recommended are products we use and love, and want to share them with you!